Ankle sprains are often a high incidence injury in any physical activity.
In padel, due to the variability of actions and sporting gestures, this incidence is usually increased compared to other sports, making it one of the most frequent injuries in padel.
An inversion ankle sprain or lateral ankle sprain is caused by a sudden movement of the foot in inversion, where the lateral ligaments of the ankle, responsible for the stabilisation of this joint,

are subjected to a sudden increase in tension beyond their physiological elongation capacities.
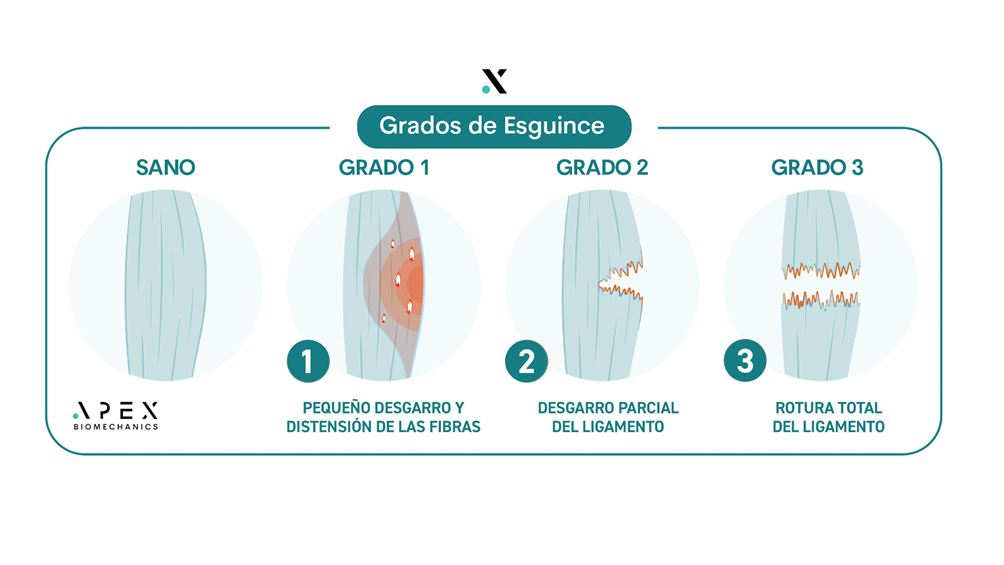
Depending on the degree of intensity of this sudden ankle inversion, we can differentiate between three types of sprains according to the degree of ligament involvement.
DEGREES OF ANKLE SPRAINS IN PADEL
Degree I sprain: A strain of the collagen fibres of the ligament is generated, with inflammation, pain on movement and compression. Generally, it is possible to walk with a certain degree of normality.
Degree II sprain: there is a partial tear of the ligament of one of the ankle ligaments, with inflammation and haematoma. It is usually painful when walking and, unlike Grade I, there is a greater exacerbation of symptoms and functional limitation.
Degree III sprain: complete rupture of a ligament with possible bone injury to the tibia, fibula and possible involvement of certain tendons and bones of the foot. More intense pain, with greater local inflammation. There may be pain in the tibia or fibula, because of injuries to these structures.
FACTORS FAVOURING ANKLE SPRAINS
There are several factors that influence the risk of an ankle sprain, among them:
– Incorrect physical preparation and lack of strength in the muscles that stabilise the ankle and our leg.
– Incorrect functioning of the foot or poor footing.
– Reduced ankle mobility.
– Having suffered previous sprains.
– Ligamentous hyperlaxity.
– Incorrect or deteriorated footwear.
HOW TO PREVENT AN ANKLE SPRAIN PLAYING PADEL?
Given that ankle sprains occur in sudden and unexpected gestures that we cannot anticipate, it is not possible to prevent them completely, but we can work on those functions that improve the strength of our musculature and its capacity to respond to a sudden stimulus such as a sprained foot, as well as eliminating those risk factors mentioned above.
In this way, we can reduce the risk of suffering an ankle sprain by following these recommendations:
- Adequate physical preparation work, incorporating exercises focused on ankle proprioception or sensorimotor work and increasing strength in the muscles that stabilise the ankle (foot and leg muscles), as well as in the structures that stabilise our body in general, such as the CORE.
- Use of specific padel shoes, suitable for the surface on which we usually play.
- Study the footprint and evaluate the use of customised insoles, especially if we suffer from repeated sprains or chronic ankle instability.
- Correct warm-up before playing a padel match.
TREATMENT WHAT TO DO IF YOU HAVE SUFFERED A SPRAINED ANKLE PLAYING PADEL?
After suffering an ankle sprain, we will differentiate the phases of treatment, where the first hours are of vital importance to avoid complications and future recurrences.
STAGE 1. FIRST 48-72H
- Assess the severity of the sprain and in case of suspicion of grade 2 or 3, go to the emergency department for an X-ray to rule out or confirm bone lesions.
- DO NOT cast or splint the foot unless the sprain is grade 3.
- It is NOT recommended to take anti-inflammatory drugs (except in cases of severe pain) as this can have a negative impact on subsequent tissue recovery.
- Apply a compressive bandage to promote absorption of the initial oedema.
- Apply ice for 5 minutes at a time.
- Support and walk despite slight pain, as this will promote absorption of the oedema and prevent reduction of mobility.
- See a physiotherapist after 48-72 hours to begin treatment of the sprain, focusing on reducing inflammation, favouring drainage of the oedema and reducing painful symptoms.
STAGE 2. From 3 to 5 DAYS
- Application of a functional bandage by the physiotherapist or indicated health professional, which will allow us to walk and even carry out physical activity in a controlled manner, without any risk to recovery or aggravation.
- Start ankle mobilisation and functional rehabilitation work. This should be prescribed by a professional. This is the most important part of the recovery from the sprain as it will help restore the ankle’s functionality so that you can return to sport as soon as possible.
- Physiotherapy treatment.
STAGE 3
- Remove the functional bandage and lead a normal life.
- If you are able to do sport, use a functional bandage or ankle brace for sporting activities.
- Continue with ankle mobilisation and functional rehabilitation work to promote ankle stability and restore the functional capacity of the ankle.
Aitor Castrillo
CEO and podiatrist Apex BiomechanicsInstagram account: @aitor.apex // @apex.biomechanic


